The Coal Workers You Didn’t Know Existed—And Why They May Be At Risk

Alfred Ray Price, who worked for 28 years in the coal industry, shown with his wife Willa. Price believes that his health problems are directly linked to the years he spent working with chemicals used to clean coal. Photo courtesy of Alfred Ray Price.
Route 3 cuts through the heart of southern West Virginia coal country, but from the road, you might not even know it. Much of the surface mining is above your head, along the ridges of the Appalachian mountains that flank the road. You’re not likely to spot the entrance to an underground mine, either, though there’s one sure way to tell a mine is nearby: the towering metal structures of coal preparation plants punctuate the landscape. Stilted conveyer belts pass over the road, carrying coal from the mines. Once the coal arrives at these plants, it’s treated with chemicals to remove impurities and prepared for sale.
Two class-action lawsuits have revealed a great deal of evidence, and some testimony, regarding chemicals at coal prep plants.
The dangers faced by coal miners have been well-documented—black lung disease, for example, was identified decades ago. But about 15.3 percent of workers in the mining industry—an estimated 10,500 people—are employed not in mines but in preparation plants, mill operations, or breakers nationwide, and evidence suggests that these prep plants pose their own dangers for those working inside.
 A variety of chemicals are used in these prep plants on a daily basis, many of them to purify coal. MCHM (4-methyl-cyclohexanemethanol), the chemical that left almost 300,000 West Virginians without safe drinking water after a spill in January, is one of these chemicals. Hundreds of people sought hospital treatment after MCHM exposure during that crisis, and at least 20 were admitted. But what are the dangers for coal preparation plant workers who are exposed to higher concentrations of these chemicals on a regular basis for the span of a career?
A variety of chemicals are used in these prep plants on a daily basis, many of them to purify coal. MCHM (4-methyl-cyclohexanemethanol), the chemical that left almost 300,000 West Virginians without safe drinking water after a spill in January, is one of these chemicals. Hundreds of people sought hospital treatment after MCHM exposure during that crisis, and at least 20 were admitted. But what are the dangers for coal preparation plant workers who are exposed to higher concentrations of these chemicals on a regular basis for the span of a career?
As with MCHM, the answer proves to be nebulous. For many of these chemicals, complete information on their potential health effects isn’t available, and long-term effects are even more difficult to establish. One workers’ rights organization, the United Mine Workers of America (UMWA), has been seeking updated regulations regarding chemical safety standards and reporting for years.
Alfred Ray Price is one of many former preparation plant workers who believe their health problems can be directly linked to their time spent around chemicals. Price worked in the coal industry for 28 years, including 19 at the Montcoal #7 Prep Plant in Raleigh County, W.V. He remembers spraying coal cars with antifreeze in the wintertime to keep the coal from sticking—32 gallons per car—while standing on a catwalk above.
“Have you ever sprayed a water hose in a bucket, and get all the mist up from it?” Price asked. “By the time I would get through spraying the cars, I would be soaking wet with it. Actually, it would be running down my throat. It was a real sweet taste.”
Price had to stop working because of health problems at age 47. He said PET scans of his brain pointed to cognitive disorders, including short-term memory loss. He later became involved in one of two class-action lawsuits in Marshall County, W.V., in which about two dozen plaintiffs claimed similar chemical exposure and health problems. Many of those plaintiffs also claimed they spent years working around chemicals without being warned they could be dangerous.
One suit was settled last year, and the other was dismissed. The settlement provides for a one-time health exam for prep plant workers—but specifies that these exams aren’t intended to determine whether any health problems may have been caused by the chemicals in question. Thomas F. Basile, attorney to several of the plaintiffs, is attempting to reinstate some of the claims in these cases, and says he’s considering an appeal in the U.S. Supreme Court.
Price and some other plaintiffs aren’t satisfied with the results, but the lawsuits did achieve one thing: they placed on public record a great deal of evidence, and some testimony, regarding chemicals at coal prep plants.
One plaintiff, Franklin Stump, told a judge that inhalation of and skin contact with chemicals was a regular occurrence at the Montcoal #7 plant, where he worked for 27 years. Much of this exposure happened during the “frothing” process, in which fuel oil and a variety of chemicals are mixed with water to create a bubbling liquid that separates fine coal particles from other materials.
“I’ve unloaded the trucks with the bags [of chemicals] in it over my shoulder, carried them up the steps, dumped them in the funnels, and it all come[s] back in your face,” Stump said, according to a court transcript. “And I’ve seen pipes bust and the stuff go all over the walls and all over your face, and I’ve waded, like I said, up to my knees.”
Price and other workers mostly spoke from their experiences in the 1990s and earlier. Phil Smith, director of communications at the UMWA, points out that at today’s newer prep plants, many processes are automated to prevent workers from mixing chemicals directly into vats of frother, thereby reducing their exposure. But workers are still exposed to these chemicals sometimes, Smith added.
So the question is, how dangerous are these chemicals, and do workers need better protection against them?
Chemicals you can find at a coal prep plant
Most chemicals used in coal preparation don’t appear too dangerous to human health, according to the Material Safety Data Sheets (MSDSs) provided in the Marshall County cases. In case you’ve never heard of MSDSs, these information sheets list chemical product contents, potential hazards, and potential health risks. They are prepared by chemical producers and are supposed to accompany any chemicals used in a workplace. The U.S. Occupational Safety and Health Administration requires that MSDSs be made “readily accessible” to employees.
But companies often withhold the exact contents or proportions of chemical mixtures as trade secrets. And that’s not the only information that’s missing; in the case of the MCHM spill, public health specialists have had a hard time proving just how dangerous (or safe) MCHM is, since not enough testing has been done to know for sure.
“We was never told or never shown any safety data sheets on it, so we could look ourselves and see what it contained.”
The Elk River spill makes the evidence presented in the two Marshall County lawsuits all the more immediate. Documents presented as evidence in the cases reveal that exposure to these chemicals—especially without the proper safety gear—can cause serious health problems ranging from pulmonary edema to central nervous system problems, birth defects, and heart problems.
In a response to a request for evidence in one of the lawsuits—Denver and Debra Pettry, et al. v. Peabody Holding Company, et al.—chemical company Cytec Industries Inc. provided MSDSs for the chemicals it had sold since December 1993 to defendants Massey Coal Services Inc., Goals Coal Company, Performance Coal Company, Bandytown Coal Company, and Elk Run Coal Company Inc.
While these documents do not constitute a complete list of the chemicals used in coal prep plants, they do offer a snapshot of the potential health hazards that prep plant workers like Price faced and still face.
 The UMWA believes updates to U.S. Mine Safety and Health Administration standards regarding these chemicals are long overdue.
The UMWA believes updates to U.S. Mine Safety and Health Administration standards regarding these chemicals are long overdue.
“We continue to see cases of cancer and other health issues due to chemical exposures,” said Dennis O’Dell, director of the UMWA’s Department of Occupational Health and Safety. “The PELs or Personal Exposure Limits have not been adjusted since the 1980s. We believe that MSHA (and OSHA) should reexamine PELs and further a study to see what occurs when workers become exposed to multiple chemical[s] at once. Right now we have MSDS material on each individual chemical, but what happens when those are all used at the same time?”
The Mine Safety and Health Administration acknowledged this point. “There are no permissible exposure limits for many of the chemicals used in coal processing,” MSHA’s Technical Support division said in response to inquiries for this article. “However, these chemicals are considered hazardous and are covered by MSHA’s Hazard Communication standards.”
On April 9, MSHA issued a health hazard alert in response to the coal processing chemical spills earlier this year. The alert reminded operators that miners and plant employees must be provided information on the chemicals they’re using.
Alpha Natural Resources (which acquired defendant Massey Coal Services Inc.) and the American Chemistry Council did not respond to interview requests. Representatives of Peabody Holding Company, BASF Corporation (which acquired defendant Ciba Specialty Chemicals Corporation), and the American Chemistry Council had no comment. OSHA did not comment on the record.
Safety precautions were ignored, workers say
During Jackie Browning’s 14 years working in coal mines, he always wore a respirator. But when the Naoma, W.V., resident started operating a bulldozer at a coal prep plant in 1991, he didn’t think he needed one any more.
Browning worked outside around the coal piles, not indoors with the frother, and he says that for the first seven years, the job didn’t seem to affect his health.
The Dangers of Polyacrylamide
While it’s difficult to assess exactly how dangerous many prep plant chemicals are, that’s especially true of a substance called polyacrylamide. For the full story on this chemical, see Appendix A.
But things changed in late 1998, when by Browning’s account, the prep plant where he worked started making more frother—and consequently, using more chemicals. He’d be bulldozing the piles of treated coal, and the fumes would come in through the heater. Browning contends that these fumes started affecting his health almost immediately; his mouth would hurt and he got the shakes. Three weeks in, Browning said he complained to his supervisor, but nothing changed.
Finally, about six weeks after his symptoms started, Browning and a coworker were rushed to the emergency room. That was his last day of work, after 29 years in the coal industry.
“The last day I worked, at noon, they brought me a respirator. It was too late for me,” he said.
Browning isn’t the only worker who claims he wasn’t told the whole story about how to be safe around chemicals in the workplace. Price and other plaintiffs in the Marshall County lawsuits say they weren’t provided with appropriate protective gear, and didn’t know for years what chemicals they were using.
“They never mentioned toxins down there, chemicals. That was never, never, never mentioned. Never had a safety meeting on that,” Browning said.
Price agrees. “We never did have no idea what [it] was,” he said, referring to many of the frothing chemicals. “We was never told or never shown any safety data sheets on it, so we could look ourselves and see what it contained.”
Failing to provide this information would be illegal. But industry representatives dispute these claims.
—-
Nancy Gravatt, senior vice president of communications for the National Mining Association, countered that prep plant employees are properly informed about the chemicals they’re using, and that MSDSs “are posted both for reading at any time and available in the event of an emergency.” She added that employees “are trained on the substances brought onto property” at these plants.
In a stress test not long after the emergency, Browning said, “I couldn’t even stand up on a treadmill.”
However, Phil Smith of the United Mine Workers said he’s not surprised that workers may not have had access to the data sheets.
“We keep our members informed about all the chemicals that are used in coal preparation plants, and if worked with properly, they’re safe,” Smith said. But, he said, he believes nonunion operations are less likely to inform their employees regarding chemicals and their safety hazards. (Employees are never required to wear safety equipment, Smith pointed out.)

The Shumates Branch Coal Sludge Dam with a coal prep plant just below the dam. Photo courtesy of Vivian Stockman / www.ohvec.orgSouthWings.org.
Employee access to data sheets isn’t the only point of contention between workers and the industry. Another question that’s difficult to answer is just how high workers’ chemical exposure really is. Gravatt said that MCHM is used at safe concentrations.
“Typical dosage rates for frothers like MCHM are less than 12 parts per million. In other words, a few hundred cubic centimeters per minute enter into 8 to 10 thousand gallons per minute of coal slurry,” Gravatt wrote in an email. This is higher than the CDC’s recommendation of no more than 1 part per million of MCHM in drinking water. But Gravatt said there’s a difference.
“Coal prep plant employees clearly are not drinking the frothing agent. These are two very different standards. It is inaccurate to mix the two,” Gravatt wrote.
Yet workers like Price claim they did inhale and ingest the chemicals they used in the frothing process.
“We ingested it, inhaled it, got it on our skin, even digested it,” Price said. “You’d be inside of a closed area and you’d stay wet with it, and we didn’t think much about it at the time until we started getting sick one by one.”
Today, Browning suffers from multiple chemical sensitivity and burning mouth syndrome. But relatively speaking, he’s doing better. For two months after his hospitalization, Browning said, his lungs burned. (He’s not a smoker.) It took almost two years for his bloodshot eyes to clear. In a stress test not long after the emergency, Browning said, “I couldn’t even stand up on a treadmill.”
Detoxification treatments (not covered by insurance) have cost Browning thousands of dollars, and his worker’s compensation claim was denied.
More information for better solutions
Given how little we know about the toxicity and health impacts of chemicals, mapping out a clear alternative is difficult.
Dr. Alan M. Ducatman of the West Virginia University School of Public Health has been fielding health questions from prep plant workers for more than two decades. He said it’s hard to determine the cause of an ailment when you don’t know what chemicals workers are exposed to in the first place.
“We should be assuming it’s deadly toxic until shown otherwise.”
As a result, few symptoms explicitly point to prep plant chemicals as their cause, Ducatman explained—and there’s no single test that can determine whether these chemicals are at the root of workers’ health problems.
The solution, Ducatman believes, is more toxicity testing for the chemicals workers are using: “People talk about how much it costs [but] the industry is making a tremendous amount of money.”
Yet the challenge of this testing isn’t just financial—it’s also a problem of logistics.
“It’s a simple case that there are millions of chemicals available. … It takes time to do these toxicity studies,” explained Dr. Timothy C. Eisele, assistant professor of chemical engineering at Michigan Tech. So the focus has been on chemicals that have already proven themselves dangerous.
But until these logistical problems have been solved, transparency and caution are essential, insisted Vernon Haltom, executive director of the nonprofit anti-mining organization Coal River Mountain Watch.
“We should be assuming it’s deadly toxic until shown otherwise, and even then not rely on one or two tests on rats 20 years ago,” Haltom said.
Dr. James G. Speight, who has worked as a chemist and consultant in the coal and oil industries for more than 45 years, agrees that caution is key.
In referencing one coal prep chemical, polyacrylamide, Speight said: “I tend to err on the side of caution and say that chemicals of that type are dangerous. They can be poisonous.”
Today, Browning has to be cautious about every chemical he uses, down to his detergent, but it’s not by choice. He’s highly sensitive to a lot of household chemicals, which can irritate his burning mouth and other symptoms.
“I was a five- and six-day worker every week. … I was an everyday man, and I worked hard,” Browning said. “If people knew what I went through—they don’t have enough money to compensate you for this stuff.”
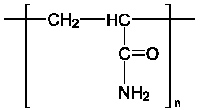
Appendix A: The dangers of polyacrylamide
While it’s difficult to assess exactly how dangerous many prep plant chemicals are, that’s especially true of a substance called polyacrylamide. At first glance, polyacrylamide doesn’t look that bad. It’s even used in cosmetics and water treatment. But polyacrylamide poses two greater dangers: first, commercial polyacrylamide often contains traces of acrylamide, the essential building block for polyacrylamide. And second, polyacrylamide also tends to break down into acrylamide.
What’s wrong with acrylamide? It may cause cancer and birth defects. One potential health impact, neurotoxicity, was first observed in laboratory animals more than 56 years ago.
A report prepared for the California Public Health Foundation in 1988 confirmed that traces of the more dangerous acrylamide are “usually present in the various bulk commercial formulations” of polyacrylamide. A representative of the American Cyanamid Company (of which Cytec is a spinoff) is on the distribution list of this report—meaning that by the time the company produced the MSDSs, all dated after 1989, it should have known that there was some acrylamide in its polyacrylamide products.
Data sheets for polyacrylamide provided in the Pettry case list minor health risks such as eye and skin irritation, but don’t mention acrylamide as a potential danger. Cytec did not respond to repeated interview requests for this article, and its attorney in the lawsuit offered no comment.
But should Cytec and other companies have to report whether acrylamide is part of its chemical mixtures? According to a the U.S. Mine Safety and Health Administration’s Technical Support division, “For mixtures, operators must list non-carcinogenic hazardous chemicals that make up 1% or more of the mixture by weight or volume and must list carcinogenic hazardous chemicals that make up 0.1 percent or more of the mixture by weight or volume.”
It’s unclear how high concentrations of acrylamide may have been in polyacrylamide products around the time of the Cytec MSDSs in question. But according to the U.S. Environmental Protection Agency, residual acrylamide concentrations have been as high as 5 percent in the past—although improvements in the treatment process through the years have reduced levels to around 0.3 percent. A 1994 EPA requirement helped spur that change.
Many more recent MSDSs for polyacrylamide, presented as evidence in the Pettry case, also do not list the presence of acrylamide. Yet at least one polyacrylamide product that Cytec sold to coal companies contained “(a) chemical(s) known in the State of California to cause cancer,” according to the MSDS. Polyacrylamide isn’t known as a carcinogen under California law, but acrylamide is. By the EPA’s standards, acrylamide remains a “probable human carcinogen,” and has been defined as such since at least 1994.
But the dangers of chemical exposure depend on how much of the chemical you’re exposed to, cautioned Dr. James G. Speight, who has worked as a chemist and consultant in the coal and oil industries for more than 45 years.
“Most people sprinkle a little salt on their food. If you eat a pound of salt, you’re going to die. It’s a question of degree,” Speight said.
Nancy Gravatt of the National Mining Association said she was not aware of the use of polyacrylamide or acrylamide at coal prep plants, and said she could not provide a list of chemicals used at such plants.
Appendix B: A battle in the courts over coal chemical transparency
Over the last decade, two class-action lawsuits in West Virginia have given a voice to coal preparation plant workers who attribute their health problems to chemical exposure in the workplace.
Today, Basile is fighting to reinstate claims in the Pettry case against Patriot Coal Corporation.
One case, Denver and Debra Pettry, et al. v. Peabody Holding Company, et al., was filed in 2002 and sought medical monitoring for prep plant and water plant workers, along with punitive damages. A similar case, William K. Stern, et al. v. Chemtall Inc., et al., was filed in 2003 and sought medical monitoring only. Both cases zeroed in on a particular chemical, polyacrylamide, whose monomer form, acrylamide, may cause cancer. The Pettry case also sought more information on other chemicals used in the prep plants.
The Pettry case claimed that the defendant chemical companies intentionally failed to warn workers of the dangers of the chemicals they were using, and that the defendant coal companies created unsafe working conditions.
Polyacrylamide is used in the “frothing” process, in which coal is separated from other minerals in order to purify it for sale.
In 2013, the Pettry case was dismissed because in most cases, plaintiffs hadn’t filed their case within the two-year statute of limitations, and because the plaintiffs’ attorney, Thomas F. Basile, had reportedly missed court dates and didn’t provide requested evidence on time. Basile, who represents some plaintiffs in both of the cases, has been fighting the decision ever since, but in January, his appeals to overturn the settlement in the Stern case and the Pettry case dismissal were turned down by the West Virginia Supreme Court of Appeals.
Basile argues these dismissals ignored the arguments or issues raised in the appeals, including requests he made in both appeals to unseal 230 pages of documents related to ethical issues, which involved conflicts of interest for lawyers in both cases.
“It’s been a long, hard, drawn-out fight, and we lost,” said Alfred Ray Price, one of the plaintiffs in the Pettry suit, in response to January’s ruling.
The Stern lawsuit appeared to have a happier ending, but many of the plaintiffs, including Price, walked away unsatisfied.
Stern reached a settlement of almost $14 million in 2013, with about half of this money allocated toward one-time medical examinations for prep plant workers, and the other half going toward attorneys’ fees and costs. Any money not used for medical testing will be donated to two West Virginia universities.
“The only ‘benefit’ provided to class members by the proposed settlement is a one-time medical examination that resembles little more than an annual medical examination that most of the class members have likely already had on more than one occasion,” Basile wrote in an email. “[And] there is no follow-up testing provided in the settlement should a medical examiner diagnose any disorder that needs further examination or consultation.”
The Stern suit sought funds for medical monitoring—but Basile, Price, and other plaintiffs insist that a one-time exam does not constitute “monitoring.”
The settlement also specifies that these exams are not designed “as a research vehicle.” In other words, they’re not intended to determine whether any health conditions discovered during these exams were caused by polyacrylamide or acrylamide.
In objecting to the settlement, Basile wrote that it “assur[es] that nothing will be learned about the types of ailments or occupational diseases suffered by those in the class who have been exposed to toxic chemicals in their work environment.”
Today, Basile is fighting to reinstate claims in the Pettry case against Patriot Coal Corporation; those claims were dismissed despite the fact that those claims were stayed while Patriot underwent bankruptcy proceedings. Basile said he is also considering an appeal in the U.S. Supreme Court.
|
Erin L. McCoy
is a former news editor and freelance reporter currently working as a public relations manager, book editor, content writer, and entrepreneur.
|