During Childbirth, Enduring the Patriarchy Was the Hardest Part

There are a wide variety of abuses that occur during childbirth because people either don’t know or don’t feel like they have options.
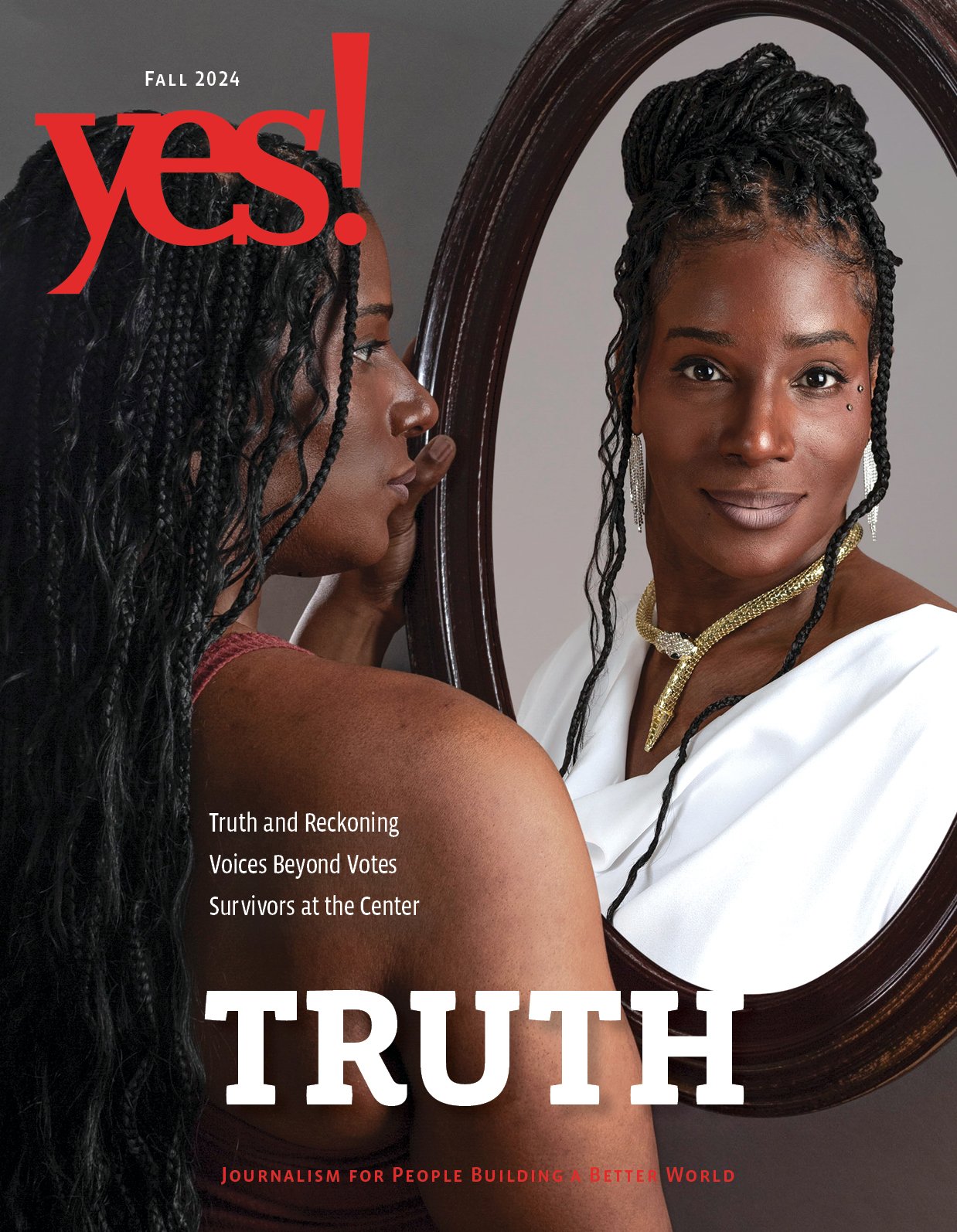
Photo by Hero Images / Getty Images.

Everyone from medical professionals to strangers tell pregnant people what they should and shouldn’t be doing with their bodies. Throughout my two pregnancies, OB-GYNs, nurses, family, and friends often used phrases like “you can’t,” “you’re not allowed to,” and “we’ll let you” when discussing my body.
Unfortunately, this is standard practice in U.S. medicine, which supports a disease-based, doctor-centered, patriarchal model of care (as opposed to patient-based care, which emphasizes collaboration, understanding, and choices). Policies and protocols are set up to avoid liability.
While in labor with my first child in 2015, I was told I couldn’t move around or go to the bathroom on my own, switch positions without assistance, or eat anything besides ice chips.
Not being able to go to the bathroom on my own was annoying; not being able to switch positions or move the way my body wanted to increased my pain. Enduring labor without eating or drinking was exhausting and directly affected my resolve to keep going without an epidural.
Pregnant people have a lot of experience being told what to do with their bodies.
It’s also just dumb. Not long after I gave birth, new research showed that food during labor was not harmful and could actually be beneficial. Sometimes new research affects medical policies, sometimes it slowly trickles down, and sometimes it doesn’t change anything.
At my second child’s birth, a nurse repeatedly told me not to scream, which I did naturally to cope with the pain. Between the contractions and labored breathing, it took me a while to protest. And when I finally did speak up, it wasn’t particularly assertive—“It’s all right, I can scream”—but it did get the nurse to stop.
When that kind of misogynistic, restrictive language is directed at you for nine months, it’s easy to forget that people (including the medical professionals you hired) may be giving you advice about your body—but that you’re the one who gets to make the decisions.
Pregnant people have a lot of experience being told what to do with their bodies. By the time they’ve made it to their first prenatal appointment, they’ve been told one or more or all of the following about their bodies in their lifetimes: They should dress it in pink; shave their legs and arm pits; keep it smooth and cellulite-free; and cover a certain amount of it most of the time and some parts of it all the time lest it send the “wrong message.”
People who become used to their bodies being policed may not have a sense of body ownership and agency. There are a wide variety of abuses that occur during childbirth because people either don’t know or don’t feel like they have options. They are coerced, given unnecessary interventions, threatened. They are denied lack of informed consent, which requires the provider to give the patient a comprehensive overview of possible risks and benefits of a treatment.
“The most pervasive language I find when dealing with pregnant people in the medical setting is coercive,” said my doula, Erin Carter, when I asked her about the language she’s encountered in medical settings. “[It’s] either meant to convince a parent that they don’t know what they know, or elicit their consent by questioning the safety of the baby (whether or not there is a safety concern at play).”
“In more progressive places, women have more freedom.”
She continued. “I have literally heard the phrase, ‘Well you don’t want a dead baby, do you?’ come out of a nurse’s mouth. … It’s ironic that I have seen this coercive language used most frequently in early labor with what would be typically considered minor medical interventions. And when clients have encountered true medical emergencies, the language used with them has more frequently been compassionate and fact-based in nature,” Carter said.
According to Cristen Pascucci, founder of organization Birth Monopoly as well as a childbirth legal rights advocate, these practices are based on the idea that the person giving birth is under the authority of the medical provider or institution.
“In more progressive places, women have more freedom, but that freedom belongs to them only as far as their care providers or institution allows it,” she said.
These normalized practices of medical bullying are now starting to get some pushback: Recent U.S. court cases that addressed abuse and coercion during childbirth include one with a physician being charged with assault and battery (based on lack of informed consent) for performing an unwanted episiotomy on a patient who repeatedly said no to the procedure, a nearly unprecedented decision. In another case, a plaintiff was awarded $16 million after receiving unnecessary medical interventions that left her permanently injured from a hospital that had advertised itself as a natural birthing environment.
After feeling pressured into a C-section during my first birth, I had more of an idea of what I would and would not allow to happen to my body during delivery. To address these decisions, I hired a midwife and doula in addition to an OB-GYN (in case I ended up at the nearest hospital, which didn’t permit midwife care) to guide me through pregnancy and birth.
Black cisgender women deal with their sexuality and reproduction being politicized.
Supported by my doctor, midwife, and doula—all women—I was kept up to date on what was going on in my body and my baby’s, given treatment options, and ultimately felt cared for. In the delivery room, everyone worked together to ensure I had a safe and successful vaginal birth after cesarean. My daughter arrived after just four hours of labor, and I felt like my body belonged to me, something I did not feel at the end of my first birth.
Unfortunately, that’s not a typical experience, especially for people of color, poor people, LGBTQ people, and disabled people, who often lack adequate access to health care that empowers them.
In the birth environment, Black women struggle for supported, healthy births. The maternal mortality rate for Black women is almost four times higher than for White women. Even when Black and White women share the same socioeconomic status, Black women are still more likely to die. Black patients are also more likely to suffer severe birth complications, be denied effective pain medication, and lack support for breastfeeding.
Black women have different language directed at them. Sherronda J. Brown, author of the essay “White Women in Robes,” explained that Black cisgender women deal with their sexuality and reproduction being politicized with stereotypes of “mammies,” “jezebels,” “sapphires,” and “welfare queens,” each of these working to construct Black women as inherently undesirable, emasculating, licentious, angry, and sexually irresponsible.
“Continually battling against words like ‘grown’ and ‘mannish’ that are inscribed upon our bodies from the time that we are children. We are muled, by everyone,” Brown said.
The language we use directly reflects the way we treat each other. The differences between my two births were largely due to the team of caregivers I assembled, all of whom practiced some form of respectful maternity care. The language used during my second birth was also much more respectful, with far less occurrences of restrictive verbiage.
Each person is the only one who gets to make decisions about their body.
Updated Nov. 3. A previous version incorrectly reported that Cristen Pascucci is the vice president of Improving Birth. She is the founder of Birth Monopoly. This version has been corrected.