From IVF to Miscarriages: 5 Ways We Can Talk About Infertility

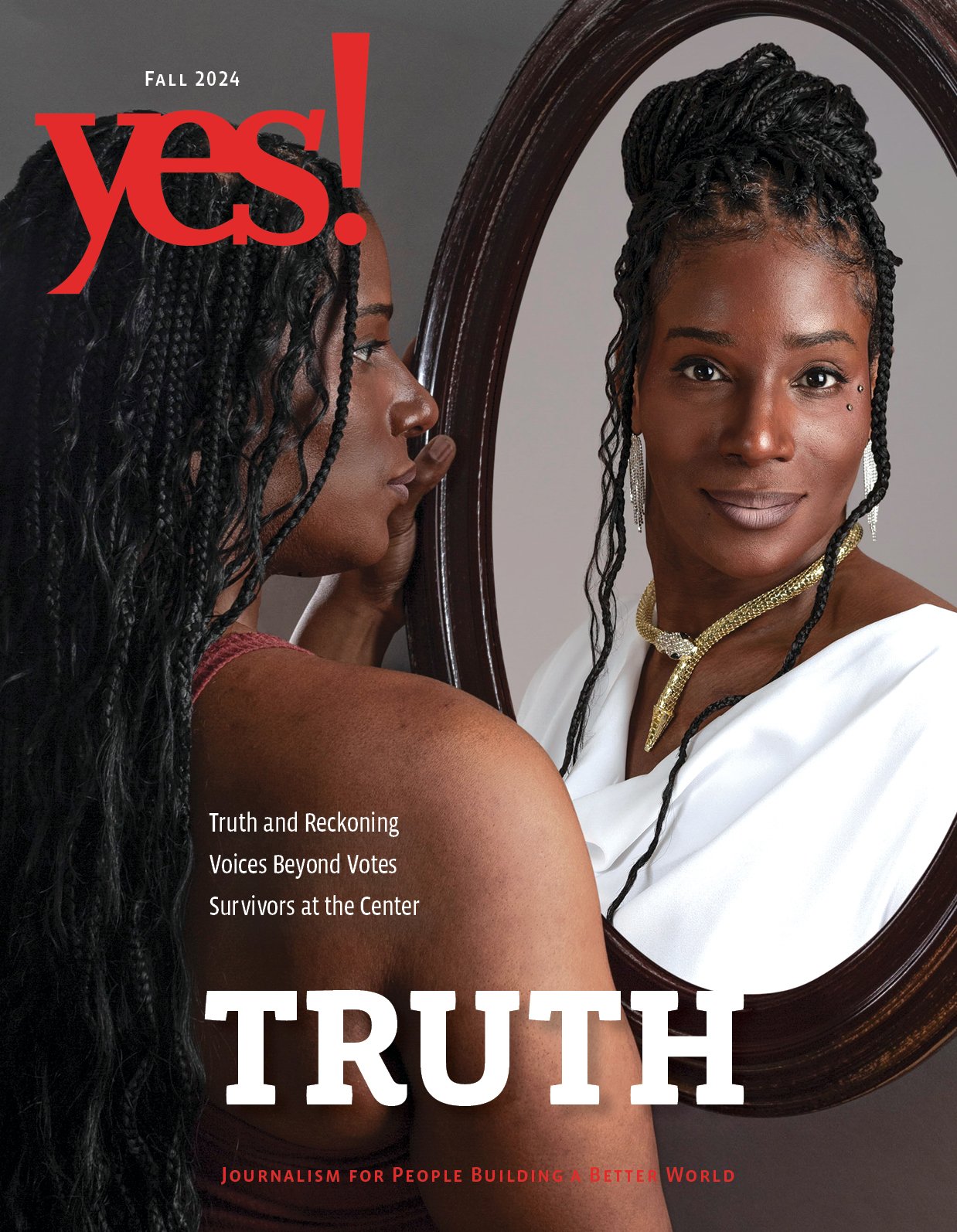
Former first lady Michelle Obama kicks off her book tour with a signing at the Seminary Co-op Bookstore on November 13, 2018, in Chicago.
Photo by Scott Olson/Getty Images
After two miscarriages at age 41, Amy Klein decided to visit a fertility clinic. It took her five clinics and four years to finally carry a pregnancy to term. And recognizing a void in conversations around fertility and information about it, she began to chronicle her experiences.
She wrote about it in a regular New York Times column, addressing her private concerns in a public way. She became the person people went to for online advice about infertility and in vitro fertilization. But Klein found that the more she wrote and talked about it, the more obvious the need for guidance and support appeared.
The reality is that despite being relatively common, infertility and the use of aids to address it are not something people talk openly about—whether out of embarrassment, lack of education, or society’s expectations of “natural conception.”
“I realized that although people are much more open about infertility, miscarriage, and IVF, women still struggle with getting through the process, from ‘Oh shoot, am I infertile?’ to … ‘How will I pay for all this?’ she says.
So Klein is writing a book, which she describes as the “A to Z Guide to Infertility.”
The emotional impact of miscarriage and infertility runs deep. And it affects all walks of life, from the woman sitting on the bus beside you to some of our most beloved figures, such as former First Lady Michelle Obama.
In her new book, Becoming, Obama lets readers into some of the darkest and most intimate moments of her life by telling about her struggles with infertility.
By sharing her experience with IVF and the role it played in the conception of daughters Malia and Sasha, Obama is helping start important national conversations about a condition many women suffer in silence.
With the launch of Obama’s book, more women are talking about IVF and infertility. Admitting it openly—in public. The result has been a recognition of how little time we allocate for those who have experienced this arduous yet life-changing procedure to share their stories.
Here are five ways we can continue these conversations.
1. Remove the stigma around infertility
Infertility is still a taboo subject. A woman’s value is deeply intertwined and connected with reproductive expectations. And the stigma surrounding it can magnify its emotional and physical consequences.
After a year of trying when she was 31, Rachael Rifkin went to see a reproductive endocrinologist. She was diagnosed with unexplained infertility. After three rounds of intrauterine insemination and one failed round of IVF, she was implanted with two fertilized eggs, resulting in her son, born in 2015.
“I felt like I should have been able to become pregnant with no issues.”
A year later, she and her husband got pregnant, unassisted. Rifkin vividly remembers the journey. “I felt like I should have been able to become pregnant with no issues,” she says. “Fertility issues happened to other people. [I felt like] something was wrong with me and my body because I couldn’t conceive.”
The taxing IVF experience coupled with social narratives that fertility and motherhood are negotiable aspects of womanhood, can lead to frustration and self-doubt. For Rifkin, those feelings of ineptitude were the hardest part.
“It could be physically uncomfortable, and the cost was stress-inducing at times,” she says. “But the emotional aspect was the worst: Feeling like something was wrong with me and/or my spouse and not believing it would ever happen.”
2. Address the physical and emotional consequences of IVF
IVF is very invasive. Egg retrievals, embryo transfers, pregnancy testing, and regular hormonal injections, which present their own challenges considering most people hate needles, can aggravate not just the body, but the mind.
Going through that process with no guarantee of success can be so grueling that many begin to wonder if it’s worth it. For women of all ages, the odds of a live birth using IVF are between 34 and 42 percent, over three cycles. The success rate for women using her own eggs declines with age.
“I think everyone gets to the point where they feel, ‘Maybe I’m not meant to be a mother, maybe I waited too long,’” Klein says. “There’s a lot of judgment against women for being selfish and focusing on their career [when] maybe they just weren’t ready to get pregnant.”
Klein recommends getting a head start on the process by not waiting too long to evaluate your reproductive status. “There are many things that can be done before starting IVF—you need to make sure you have a thorough health workup of your hormones, uterus, and tubes, sperm [if partnered], to see if you can get pregnant naturally, before starting treatment,” she explains.
3. Discuss the undue financial burden of IVF
Infertility can be expensive. Not all treatment are covered by insurance.
“Between doctor visits, the procedure to extract eggs and then fertilize them, and fertility medicine, it was around $20,000,” Rifkin says. “We were able to pay for the IUIs and some of the IVF and got help from family for the rest.”
Others like Klein had an even more costly experience. “I’d say it cost nearly $50,000—and we even went abroad for free IVF, though that cost us in work lost and travel,” she explains.
The lack of insurance coverage can make infertility seem like a personal deficit, which of course reinforces the shame.
When we discuss reproductive assistance, it’s vital that we highlight the cost as well. According to the CDC, only 15 states have enacted legislation requiring private insurance pay all or some of the cost of infertility treatments and only eight require reimbursement.
However, in most circumstances, IVF is not covered by insurance. That lack of coverage can make infertility seem like a personal deficit, which reinforces the shame.
By discussing the cost, we can address the undue financial burden fertility assistance places on families and look at the way class can be a barrier to family planning for more disadvantaged groups.
4. Acknowledge race-related disparities
Infertility narratives regularly highlight the experiences of wealthy, White straight couples. But while our depictions of infertility and IVF may discriminate, infertility does not. Like most things, race must be considered when discussing outcomes.
“There are a number of obstacles that stand between Black women and IVF usage such as stereotyped beliefs, cultural expectations about strong, self-reliant Black women, religion/theological interpretations, cost, mistrust of physicians and medical institutions, access, awareness, and acceptance,” says the Rev. Dr. Stacey Edwards-Dunn, founder and president of Fertility for Colored Girls.
According to a study, Black women had a 14 percent lower live birth rate than White women.
Fertility for Colored Girls is one of few culturally tailored organizations seeking to improve outcomes with infertility issues by providing education, awareness, support, and encouragement for African American women and couples struggling with infertility.
Organizations such as Fertility for Colored Girls are important because research suggests Black women have lower rates of success with IVF than White women. According to a study presented in October at the American Society for Reproductive Medicine conference in Denver, Black women had a 14 percent lower live birth rate than White women.
“I think in order for Black women, in particular, to experience greater success with IVF, clinical trials and research will have to be focused not only on the unique experiences of Black women, but also focus on the implications of our physiological and genetic uniqueness as well,” Edwards-Dunn says.
5. Consider the political implications
Reproduction is a complicated process and assistive reproductive technology should be a core aspect of comprehensive sex education
Various factors—age, health, and orientation—all affect the likelihood of a woman becoming pregnant. Not discussing the social politics related to reproductive assistance increases access issues.
Monica is a Black woman who is in a same-sex marriage and lives in a conservative part of the country. (For that reason she asked that her real name not be used.) She found the IVF experience to be marginalizing as one fertility clinic after another rejected her and spouse, until they finally found one willing to work with them.
We need to start seeing challenges as a natural and normal part of the journey to parenthood.
Even though she was an organizer for a national reproductive freedom organization at the time, her employer did not provide coverage for same-sex couples obtaining support for reproductive choices. She and her partner were told that their choice to be in same-sex relationship was the reason for their conception problem.
The couple paid for two rounds of IVF with a sperm donor, using their health savings account until the money ran out.
“It was emotionally taxing and shame-inducing to constantly meet barriers to care and experience direct financial and medical discrimination as a result of systemic homophobia,” Monica says. “We also face intense racism because I am Black and my wife is White and nonbinary,” she says.
When we stop oversimplifying the process of reproduction, we will reduce the deficit-based narratives around individuals and couples who need help. We need to start seeing challenges as a natural and normal part of the journey to parenthood.
Corrected: December 7, 2018.
This version reflects that “A to Z Guide to Infertility” is a description, not the title, of Amy Klein’s forthcoming book.

|
A. Rochaun Meadows-Fernandez
is an award-winning writer, speaker, and activist working to amplify Black women's voices in the mainstream dialogue, especially within conversations on health and parenting. In addition to YES! her work has been featured in The New York Times, The Washington Post, Fast Company, and a host of other publications. She is also the founder of the #FreeBlackMotherhood movement. She can be reached at amfcontent.com for business inquiries and on social media for social connections.
|