The Good Money Issue: Solutions We Love
- For Cookbook Author, Food Is an Ally Against Dementia
- Share

Over the past several years, Paula Wolfert has been investigating if and how diet can keep dementia symptoms at bay. She stays current with the latest brain health studies and consults with her neurologist, a naturopath, and leaders in the dementia community.
Photo by Eric Wolfinger/Getty Images
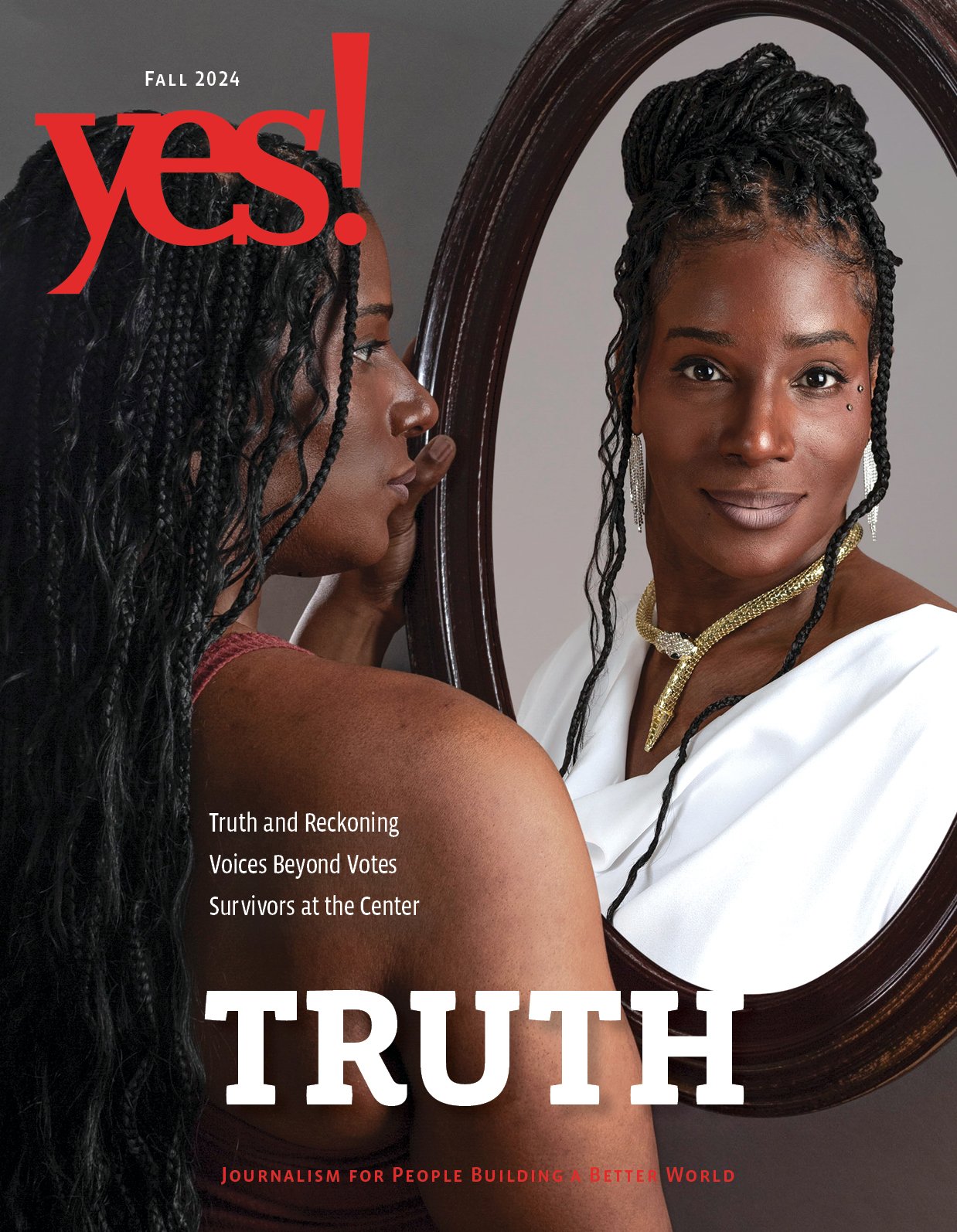
For Cookbook Author, Food Is an Ally Against Dementia
She can’t remember recipes, and food doesn’t taste the same, but Paula Wolfert believes that what she eats is key to helping her slow her cognitive decline.
Five years ago, Paula Wolfert suddenly couldn’t remember how to make an omelet as she walked into her kitchen to prepare one.
This would be unsettling for anyone who likes to cook, but for 50 years Wolfert was a leader in the culinary world, having popularized Mediterranean and North African cuisines in the United States. Wolfert had published eight award-winning cookbooks and hundreds of articles. Her culinary adventures were captured in a 2016 book called Unforgettable. In Alice Waters’ foreword to the book, she acknowledged Wolfert’s mastery: “Every element was thoroughly researched and thought out, tested over and over, clearly and logically recorded, and beautifully executed.”
Wolfert’s omelet problem, she found out, was because of a rare form of dementia, posterior cortical atrophy, similar to Alzheimer’s disease.
Now 80, she is fighting dementia with the same ferocity that she applied to studying the intricacies of French cassoulet and Moroccan couscous. Her primary weapon is what she knows best—food.
She follows a strict daily regimen involving nutrient-dense foods, nutrition supplements, and intermittent fasting, along with physical activity, a focused sleep routine, and scheduled social engagement. She keeps up on the latest brain health studies and consults with her neurologist, a naturopath, and leaders in the dementia community.
She believes that her changed lifestyle has helped slow her cognitive decline and given her a measure of control. And she resists the stigma associated with dementia.
“I don’t have any shame about this disease,” she says. “It’s not my fault. Too many people get scared of what having the disease means and what other people will think. They deny, and they hide.” Wolfert prefers to be open. She willingly shares her story and was a spokesperson for the Alzheimer’s Association.
“No cure”—then what?
Dementia is a term for a variety of disorders related to mental decline from damage to the brain’s nerve cells. It affects memory, language skills, judgment, and comprehension, among other functions. Though it usually occurs in older people, contrary to common belief, dementia is not a normal part of aging. There is no cure.
According to the Alzheimer’s Association, 5.7 million Americans are living with Alzheimer’s, and the disease makes up about 60 to 80 percent of all dementia cases in the U.S.
Though lifestyle efforts are promoted to reduce the risk of Alzheimer’s, research is still at early stages for whether they can help those with the disease.
Increasingly, people are exploring self-care options such as diet and exercise to ward off or lessen the severity of other mental health issues as well, such as anxiety and depression.
Why are so many people pursuing their own solutions?
Dr. Dean Sherzai and his wife, Ayesha, both neurologists, are the co-directors of the Alzheimer’s Prevention Program at Loma Linda Medical Center and authors of The Alzheimer’s Solution. “Billions of dollars have been spent chasing brain molecules and medications to solve the problem, [yet] in 2018, we’re still no closer to a solution,” Dean Sherzai says.
Doctors like the Sherzais and many patients believe that the common medical protocol is flawed: Once a patient is diagnosed with Alzheimer’s or other forms of progressive degenerative dementia, he or she is essentially told to “settle your affairs, quit your job, and accept your fate,” says Kate Swaffer, the CEO of Dementia Alliance International, a support and advocacy group.
Swaffer, 59, is the author of What the Hell Happened to My Brain? She was diagnosed 10 years ago with a type of dementia that is now called the semantic variant of primary progressive aphasia. She says that when she was first diagnosed, there were no drugs for it. “Instead of saying to me ‘Be as well as possible,’ they just basically told me to go home and die. I wasn’t referred to anyone for follow-up care.”
She says the medical industry’s focus on a pharma cure rather than patient care left her alarmed and adrift, and it still happens to patients today.
Monica Moreno, the senior director of care and support for the Alzheimer’s Association agrees that more work needs to be done to help patients live a positive, productive life with Alzheimer’s. A small stride was made in January, when Medicare began allowing care that includes planning “life after an Alzheimer’s diagnosis.”
Committing to a new way of life
Without much medical guidance, people with dementia and their caregivers are left to figure things out for themselves.
Wolfert did. And Swaffer devised her own plan after researching and consulting a nurse, a new neurologist, and health care practitioners familiar with helping people recover from a brain injury. Swaffer also eats a limited diet and uses meditation to help with her focus, mood, and pain. She also participates in cognitive and physical rehabilitation and works with a naturopath for supplements and ayurvedic treatments.
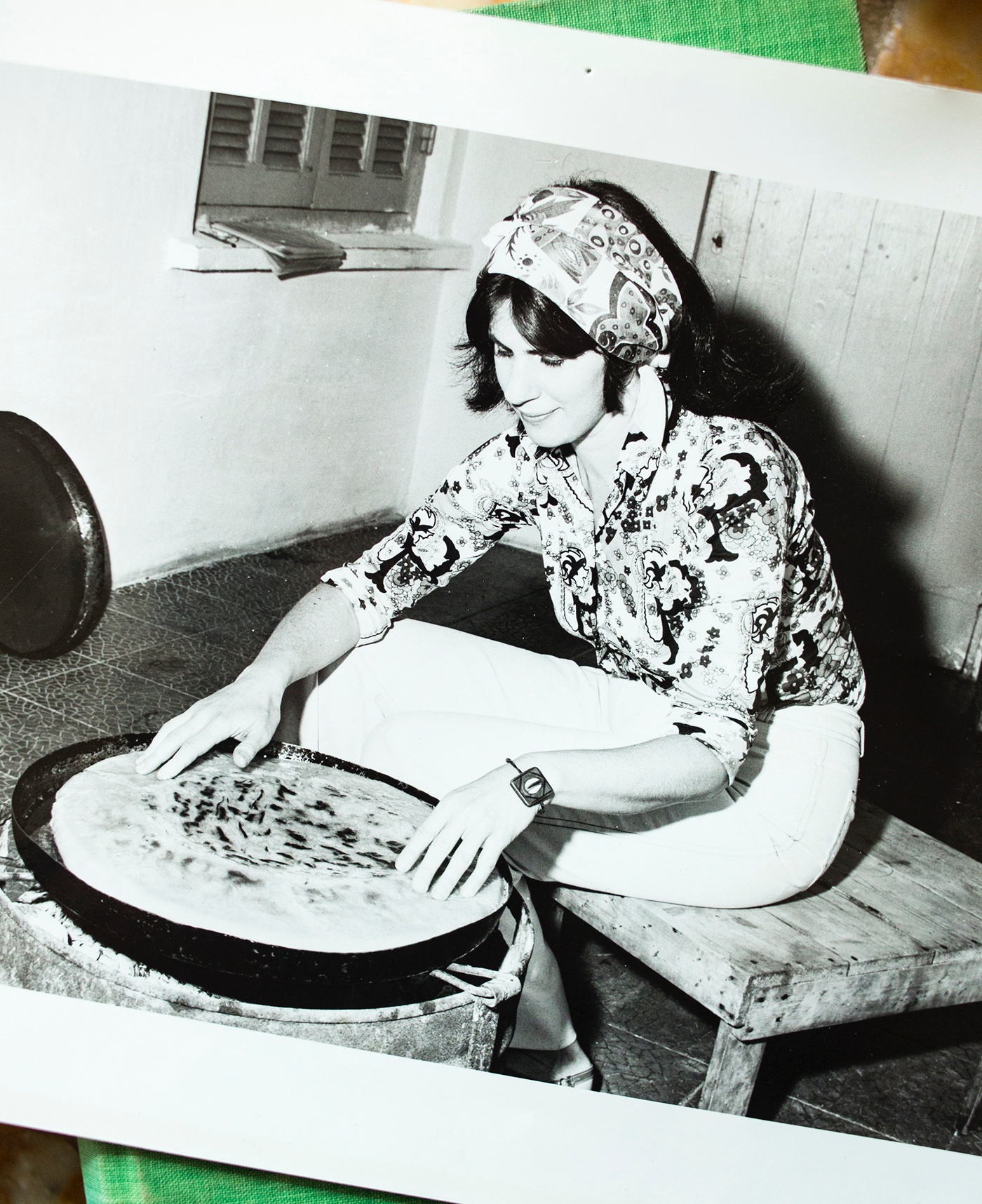
A snapshot of Paula Wolfert in the 1970s. She authored eight influential cookbooks exploring for American audiences the flavors of Morocco France and the Mediterranean. Photo by Eric Wolfinger/Getty Images
“The lifestyle changes I made haven’t cured me, but they definitely have slowed the progression of the disease,” Swaffer says.
One of the other key tenets of the advocacy group is peer-to-peer support. “We are the experts of the lived experience of dementia,” Swaffer says. Socializing and laughing together and sharing resources are fundamental for people to help deal with the sometimes-frightening symptoms they face. Social interaction not only helps a person’s emotional state but brain function as well. Wolfert and Swaffer each host several support groups, and many online outlets are also available: the 26,000-member Alzheimer’s and Dementia Support Group on Facebook, the Alzheimer’s Association’s ALZConnected, and the ApoE4 forum for people with high genetic risk for Alzheimer’s disease.
Can dementia be “reversed”?
In the forums and group talks members may swap stories on the best form of magnesium for brain health or research on cannabis for better sleep.
And they talk about the Bredesen Protocol.
Dr. Dale Bredesen’s work has been one of the more buzzed-about topics in recent years because he says he has reversed Alzheimer’s cognitive decline in his patients. He is a professor and the founding president of the Buck Institute for Research on Aging and the author of The End of Alzheimer’s. He has been studying degenerative brain disorders for 30 years.
Bredesen says that the medical community hasn’t solved the dementia puzzle because the focus on a drug fix is an oversimplified approach. “That’s like trying to apply a checkers strategy to a chess match,” he says. “What are the root causes for the problem?’”
Dementia is complex. “Most people have at least 10 or up to 25 contributing factors, such as inflammation, exposure to toxins, insulin resistance, too much stress, hormonal imbalances, genetics, nutrition deficiency, gut microbiome imbalance,” among others. He believes the key to figuring out how to stop progressive brain deterioration is to identify the unique triggers for each person and make changes to correct their imbalances.
His approach is controversial. Opponents say that his testing and lifestyle protocols can be expensive and too rigid for many people to follow.
Although the Sherzais don’t mention Bredesen by name, they say that, based on their own clinical research, lifestyle changes may slow down the progression or even prevent the development of Alzheimer’s. But whether it reverses the disease has not been clinically proved. Suggesting that it has, they say, creates unrealistic expectations for patients.
Bredesen says, “I completely understand that we don’t want to give people false hope. But people have been given a false sense of doom.”
A new relationship with food
There’s no sense of doom in Wolfert, even though her condition has basically cleared her prized palate. “I’ve lost my sense of taste. I have absolutely no memory of the taste of foods or the names of foods.”
After decades of eating and cooking around the world, she’s now making food work for her in a different way.
What does she eat now?
“I believe in the Mediterranean diet; I ate it for 50 years. It helps, but it isn’t all great.” She now mostly follows a Ketoflex 12/3 diet, which means eating a plant-based, high-fiber, healthy-fat diet within a 12-hour window and avoiding eating at least three hours before bed. Though research is inconclusive, studies have shown that with the diet’s (good) high-fat, low-carb focus, the body converts fat into energy (as fatty acids and ketone bodies). The ketone bodies can pass the blood-brain barrier and may serve as a restorative energy source for the brain.
She says that six days a week, “I only make one meal a day, around 1 p.m. For the seventh day I go out with three or four women. It’s a ritual. I’ve been going to my lunch on Tuesdays for 14 years.”
She eats mostly vegetables and, occasionally, pasture-raised eggs and meats and wild-caught fish. “I miss carbs. I miss bread and potatoes, but I’ve gotten over it.” When she does cook, she tries easy dishes, sometimes with her son. “We cook Asian food together because he loves it.” Also “because I can taste them. I can’t taste ketchup, but I can taste sriracha!”
Not Bad Pad Thai is one of her new regular recipes. It comes from Dr. Steven Gundry’s The Plant Paradox. “I made it one day for my husband, Bill. He said, ‘I want this every week.’ So, I make it every Saturday.”
Gundry is another of her favorite resources. The founder of the Center for Restorative Medicine has written several books on how to avoid illness through diet. He believes “disease begins and ends in the gut” and advocates for nutrient-dense foods and increasing the balance of good bacteria in the body’s microbiome.
“This is how it is now,” Wolfert says. “If someone said tomorrow that there was a pill cure, if I trusted the doctor, I would take a pill. For now, there isn’t.”
Despite what some might see as a dramatic shift in her relationship with food, Wolfert at times can seem gleeful. “How you feel on this program is fabulous, once you get used to it,” she says.
And here’s something she still remembers: Her grandmother told her when she was a young girl during World War II, “You can’t win a war unless you’re willing to fight.”
|
Linda Ingroia
is a food and health editor and writer. She was formerly executive editor at Houghton Mifflin Harcourt.
|